

1 However, there are mixed opinions on the efficacy of such changes. The aim of the regulation was to address fatigued residents and reduce medical errors by tracking maximal weekly work hours, shift length durations and total hours worked monthly for all residents. The Accreditation Council for Graduate Medical Education (ACGME) instituted the implementation of 80-hour workweek restrictions for residents in 2003. Adherence to work hour guidelines is essential for resident wellbeing and a healthy and conducive clinical learning environment without diminishing operative experience. Reduction in work hour violations can be achieved with a reliable schedule, promotion of accurate reporting by residents, and monitoring through EHR reports. Over the three years since the changes, the board pass rates have improved from 64% to 80% in Certifying Examination (CE) (N = 8, Passing % non-EHR = 64%, EHR = 80%) ( p = 0.03) Qualifying Examination (QE) (N = 8, Passing % non-EHR = 100%, EHR = 93%) ( p = 0.1). No decrease in operative volume was noted for graduating residents (N = 8, non-EHR = 1062, Mean EHR = 1110) ( p = 0.5). Case volumes and board pass rates were a central focus throughout the changes. ResultsĬompared with the non-EHR era (2013–2015), the number of violations during the EHR era decreased significantly (mean non-EHR = 167.3, EHR = 24.6) ( p = 0.0009). This project also evaluated the overall cultural change and satisfaction with the program using ACGME survey data. The secondary outcomes were the residents’ comparative academic and clinical performances. The primary outcome of this project was the number of resident violations to the 80-hour rule before and after implementation of those measures. During each 4-week rotation, residents were assigned one Friday call, one Saturday call and four hours of transitional call. With the design, residents were scheduled to work a maximum of 13 hours per day beginning at 0600 and operating room (OR) time concluding by 1700. The hours are actively monitored in the residency management software, New-Innovations, and cumulative weekly reports were created. This quality improvement project evaluated the effectiveness of compliance to the 80-hour work rule in a single rural surgical training residency program with the aid of EHR.

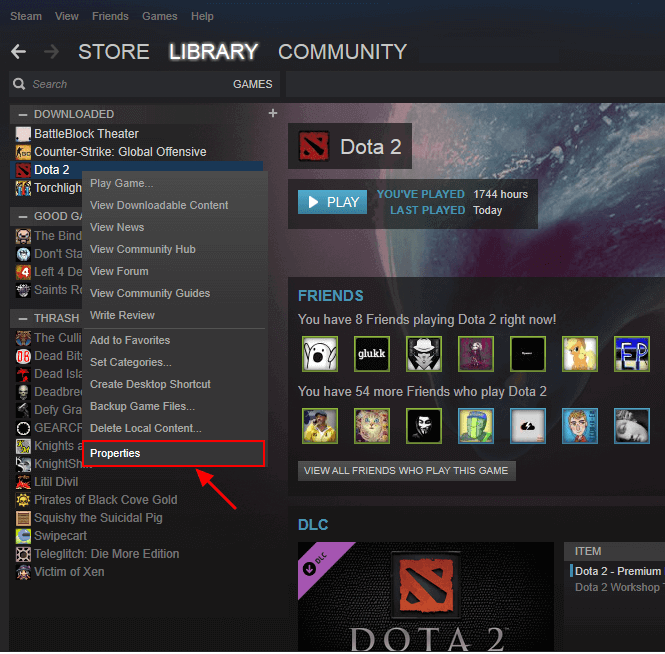
#FMINER MODIFY DOWNLOADED FILES SOFTWARE#
Reporting of work hours in the residency management software was authenticated by the organizational electronic health record (EHR). To restore accreditation requirements and provide trainees with a balanced learning environment, work hours were restructured. This resulted in multiple citations from the Accreditation Council for Graduate Medical Education (ACGME) with subsequent probation. In our free-standing general surgery residency program, it was noted over the past decade that we had an exorbitant number of resident work hours violations.


 0 kommentar(er)
0 kommentar(er)
